Credentialing in healthcare is the process that verifies the qualifications of healthcare professionals and confirms they are authorized to provide care. This involves checking education, training, licensure, and professional experience to ensure compliance with legal and professional standards. Healthcare facilities use this system to maintain high standards and protect patient safety. Effective credentialing ensures that patients receive care from highly qualified providers.
This process includes numerous steps, such as primary source verification and obtaining necessary certifications. By doing so, healthcare organizations can mitigate risks and foster trust with patients. The importance of credentialing can’t be overstated in today’s healthcare environment. It not only supports compliance with regulations but also enhances the credibility of healthcare facilities. Through tools like specialized software, the credentialing process can be streamlined, making it easier and more efficient for healthcare providers.
Purpose of Credentialing in Healthcare
Credentialing plays a critical role in maintaining quality care and ensuring patient safety. Two major purposes of credentialing in healthcare are:
Ensuring Quality and Compliance
Credentialing verifies the qualifications and training of healthcare professionals. By assessing their education, licensure, and certifications, it ensures that only qualified providers deliver care. This helps reduce medical errors and improve patient safety by ensuring staff are competent and knowledgeable. Credentialing fosters a culture of accountability by meeting regulatory and industry standards, boosting the reputation and trustworthiness of healthcare providers and institutions.
Mitigating Legal and Financial Risks
Credentialing helps minimize legal and financial risks for healthcare organizations. By validating staff competence, it reduces the likelihood of malpractice claims and legal issues. Ensuring that all providers meet required standards helps avoid potential penalties and legal consequences.
Healthcare facilities benefit financially from credentialing as well. It lowers insurance costs by reducing risks associated with unqualified staff. Credentialing also facilitates smoother operations and coordination within the organization, leading to better overall efficiency and reduced liabilities.
Effective credentialing serves as a safeguard against potential risks, protecting both patients and healthcare organizations. It ensures that healthcare providers are competent, reliable, and following best practices, ultimately leading to safer and more efficient care for all.
Types of Credentialing in Healthcare
Credentialing in healthcare is essential for maintaining high standards. It ensures that healthcare professionals possess the needed qualifications and skills. This section covers the important aspects of primary source verification, payer enrollment, and privileging.
Primary Source Verification
Primary source verification is a key step in healthcare credentialing. It involves confirming the professional’s qualifications directly from the original source. This includes verification of education, training, licensure, and certifications. For example, when a doctor claims to have graduated from a certain medical school, the credentialing team contacts that school directly to confirm. This process reduces the risk of fraud and ensures accuracy. It also involves checking for any disciplinary actions or malpractice history.
Agencies like hospitals and health plans typically perform this verification. Tools and repositories, such as state medical boards and the American Medical Association, play a significant role in this process. Overall, primary source verification ensures that only qualified professionals deliver patient care.
Payer Enrollment
Payer enrollment enables healthcare professionals to be included in insurance networks. This process is necessary for providers to receive payment for services rendered to insured patients. The process starts with the submission of detailed information about the provider’s credentials to the payer. This includes verifying licenses, liability insurance, and education history. After submission, the payer reviews and approves the application, making the provider an in-network provider.
Being enrolled in payer networks is vital for healthcare professionals to expand their practice and reach more patients. It assures patients that their insurer recognizes and covers services from these providers. Without payer enrollment, providers might struggle to receive proper reimbursement for their services.
Privileging
Privileging grants a healthcare provider the authority to perform specific procedures and offer certain services within a healthcare facility. This process ensures that the provider is skilled and competent in the specific area they are being privileged for. The process begins once primary source verification is completed. Then, the healthcare facility reviews the provider’s experience and competence in the specific procedures. For instance, a surgeon must demonstrate their skill and experience to be privileged to perform surgeries in a hospital.
Regular re-evaluation is also part of privileging to maintain high standards. Hospitals and clinics typically handle this process internally. Privileging is crucial in ensuring that patients receive care from providers who are both qualified and proficient in the necessary procedures.
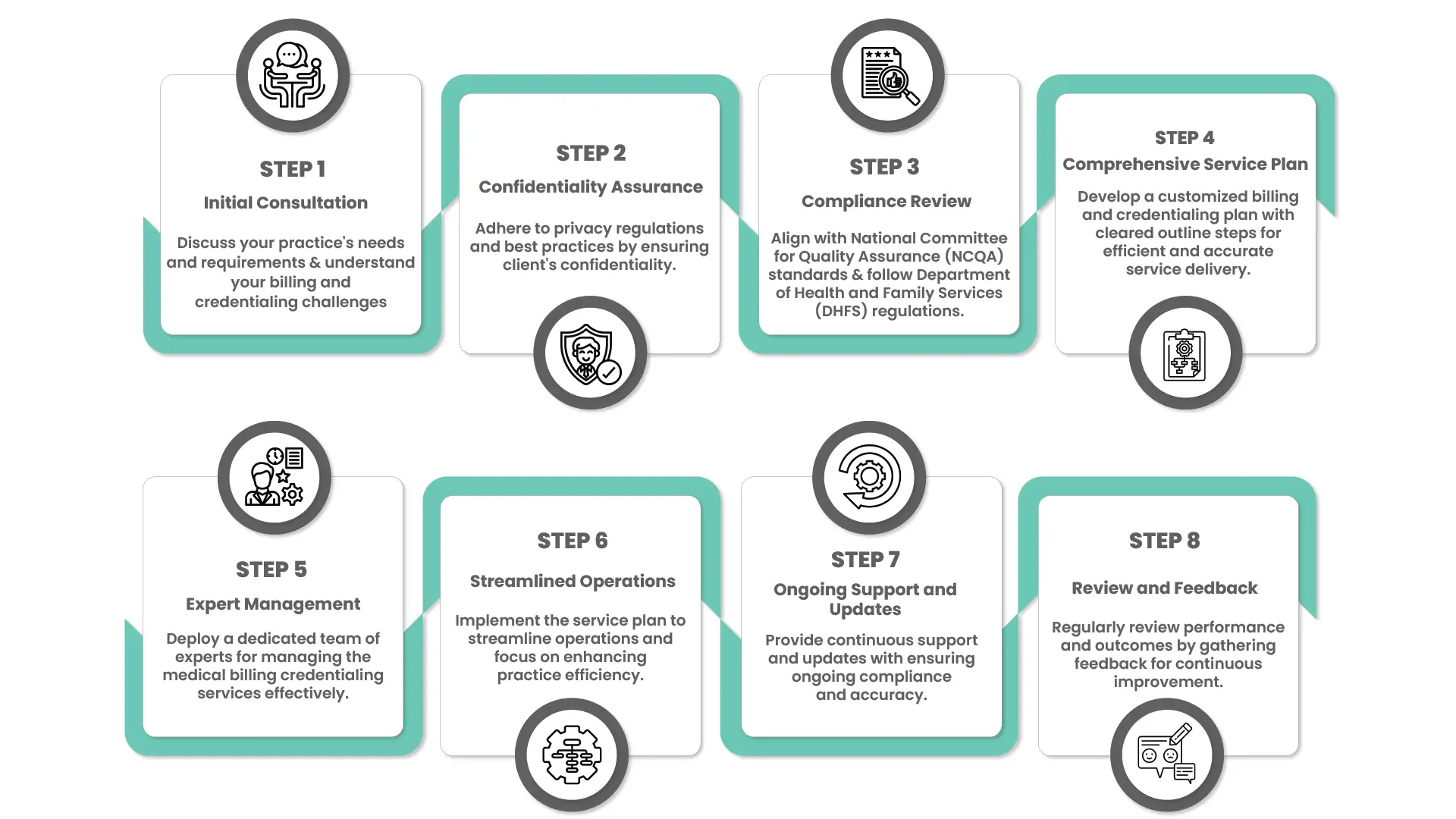
Steps of the Credentialing Process in Healthcare
The credentialing process involves several steps including gathering documentation, verifying credentials, reviewing applications, and monitoring ongoing qualifications. For a detailed flowchart of the process, you can refer to our Credentialing Process Flow Chart.
Benefits of Credentialing in Healthcare
Credentialing offers numerous benefits that help maintain quality care and ensure patient safety:
- Improved Patient Safety: Ensures that only qualified and competent healthcare providers deliver care, reducing medical errors and enhancing patient safety.
- Regulatory Compliance: Helps healthcare organizations comply with industry standards and regulations, avoiding legal penalties and enhancing credibility.
- Risk Management: Reduces the likelihood of malpractice claims and other legal issues, thereby protecting the organization from potential risks.
- Operational Efficiency: Streamlines the hiring process and ensures that healthcare providers are competent and reliable, leading to better coordination and efficiency within the organization.
Delegated Credentialing in Healthcare
Delegated credentialing involves shifting the responsibility for the credentials verification from one healthcare entity to another. This process affects various aspects such as efficiency and accountability within healthcare systems.
Understanding Delegated Credentialing
Delegated credentialing occurs when a healthcare entity, such as a hospital or health system, is granted the authority to evaluate and verify the qualifications of healthcare practitioners on behalf of another entity, often a payor like a Preferred Provider Organization (PPO). This means the delegated entity not only verifies credentials but also makes credentialing decisions. This system is designed to streamline workflows and reduce administrative overhead.
The Role of Managed Care Organizations
Managed care organizations (MCOs) play a significant role in delegated credentialing. They often delegate credentialing tasks to large health systems to manage the process internally. By doing this, MCOs can focus on broader aspects of care management. The health systems, now acting as credentialing entities, have to comply with standards set by organizations such as NCQA, URAC, or CMS. This compliance ensures that the credentialing process remains rigorous and trustworthy.
Advantages and Challenges
Delegated credentialing offers several advantages, such as improved efficiency and reduced administrative burden for the delegating entity. Health systems can streamline credentialing policies to meet multiple compliance standards, thereby enhancing operational efficiency. However, the process comes with challenges. Ensuring consistent compliance and managing the added responsibility of credentialing can be complex. If not managed well, it could lead to potential risks in credentialing accuracy.
Delegated credentialing is a nuanced topic in healthcare, directly impacting operational efficiency and accountability in managing healthcare provider credentials.
Credentialing Technology and Innovation
Advancements in technology are transforming the credentialing process, making it more efficient and reliable. Software solutions and emerging technologies like blockchain and artificial intelligence (AI) are playing crucial roles in these changes.
Credentialing Software Solutions
Modern credentialing software helps healthcare organizations manage the credentials of their providers efficiently. These platforms automate much of the manual work involved, reducing the time and effort needed to verify and maintain records. Using credentialing software, organizations can easily track expiration dates, renewals, and compliance requirements. This improves accuracy and reduces the risk of human error.
Key features often include:
- Automated alerts for upcoming credential renewals
- Digital document storage and retrieval
- Real-time status tracking of credentialing applications
Companies offers technology platforms that streamline these processes, helping large health tech companies and hospitals manage their credentialing needs efficiently.
The Impact of Blockchain and AI
Blockchain technology offers a secure and transparent method for credential verification. It allows all parties to access and verify credentials, reducing the time needed for background checks and decreasing the potential for fraud. Distributed ledger technology can also facilitate collaboration among different healthcare organizations, enabling them to share verified information seamlessly.
Artificial intelligence (AI) adds another layer of efficiency by automating data entry and verification processes. AI tools can quickly analyze vast amounts of data, identifying discrepancies and ensuring accuracy. These innovations not only save time but also significantly cut down the costs associated with credentialing. By adopting these technologies, healthcare organizations can ensure safety and compliance while focusing on providing quality care.
Frequently Asked Questions
Credentialing is the process of verifying the qualifications, training, and experience of healthcare providers to ensure they meet the required standards to deliver care. Privileging is the process of granting a healthcare provider the authority to perform specific procedures and offer certain services within a healthcare facility, based on demonstrated competence in those areas.
Healthcare professionals typically need to be re-credentialed every two to three years. This process involves updating their information and undergoing another review to ensure they continue to meet the necessary qualifications and standards.
Credentialing involves verifying a healthcare provider’s qualifications, including education, training, and work experience. Organizations use primary source verification, which means they contact the issuing institutions directly. This process ensures that all credentials are authentic and up-to-date.
In a hospital, the credentialing process is usually managed by the medical staff office or the human resources department. Credentialing specialists and coordinators are responsible for collecting and verifying the necessary documentation, performing primary source verification, and ensuring compliance with regulatory standards. The credentialing committee, composed of experienced medical professionals, reviews and approves the credentialing applications.
Credentialing in healthcare includes verifying licenses, certifications, and special training. There are also checks for malpractice history and criminal background. Each organization might have specific requirements, but maintaining updated records is a common necessity.
The credentialing process can take anywhere from a few weeks to several months, depending on the complexity of the verification process and the responsiveness of the issuing institutions. On average, it takes about 60 to 90 days to complete the credentialing process for a healthcare provider.
Credentialing ensures healthcare professionals meet established standards, which helps maintain quality and safety in patient care. It prevents unqualified individuals from practicing and ensures that ongoing education and skill development are verified.
A healthcare credentialing specialist collects and verifies data from providers. They communicate with educational institutions and licensing boards. They also ensure all documentation is complete and meets the necessary criteria before granting privileges to work.
Credentialing affects medical billing by ensuring that providers are authorized to bill insurance companies. If providers are not properly credentialed, claims can be denied. This can disrupt revenue cycles and delay payments to healthcare organizations.
The checklist typically includes your professional license, proof of malpractice insurance, education and training certificates, references, and background check information. Keeping these documents updated and organized can facilitate a quicker credentialing process.