Credentialing in healthcare is a complex process of reviewing and evaluating the credibility of healthcare practitioners to fit the standard set by the government. Even though credentialing plays a critical role in patient safety and compliance, it faces challenges that affect the effectiveness and quality of services that providers Plymouth provides. Here, the author discusses recurring problems encountered in credentialing healthcare, their consequences, and methods of solving them.
What is a Credentialing Issue in Healthcare?
Healthcare credentialing issues could occur each time there is an issue during the process of verification of qualifications, training certification, licensure, or experience of a healthcare provider. These problems can cause practicing providers delays, compromise patient safety, or create non-compliance with regulations. Some sample issues are missing documentation, slow processing of the verification process, and inconsistencies in provider details. Responding to these problems timely makes sure that there is no strain on patient care and that the corporations – related to healthcare – stay within the legal framework.
Common Credentialing Issues in Healthcare
Credentialing Issue | Description | Impact |
Delays in Credentialing | Complexity arises from the lengthy processing of applications, especially those that may be half-baked or slow verification. | This implies a delay in the provider practice, hence complicating the delivery of quality patient care. |
Inaccurate or Incomplete Information | Failure and negligence, and omission in applications | Failed or denied applications in credentialing |
Payer-Specific Requirements | Standards that are different from one insurance payer to another | Payment rejections or slow contributions |
Compliance Risks | Non-compliance to regulation | Legal problems and sanctions |
Missed Renewal Deadlines | Failure to adhere to the laid down schedule for re-credentialing | Lack of privileges and forgone revenue |
1. Delays in Credentialing in Healthcare
Another common issue is that credentialing takes a very long time to complete. The process, which can take months, is often delayed by:
- Incomplete applications and or applications with wrong information.
- Delay by educational institutions or licensing boards.
- Poor funding of credentialing program, so there is a long timeline for credentialing.
These delays may in a number of cases hinder a provider from practicing, thus denying patient a chance to access care and at the same time being a source of revenue losses to the healthcare stakeholders.
2. Inaccurate or Incomplete Credentialing Information
It is equally important to note that mistakes or oversights when filling out credentialing applications are likely to result in otherwise devastating strikes or flat rejection. Fluctuations in employment records applications can lead to setbacks or outright rejections. Common issues include:
- Outdated Contact Details
- Missing Documentation
- Inconsistencies in Employment History
To address these problems, advanced training of personnel and the development of effective verification tools are to be encouraged.
3. Navigating Payer-Specific Credentialing Requirements
Credentials of insurance are difficult to standardize because different insurance payers have differences in their credentialing. Entering wrong data could lead to delay or rejection, which compilers impact healthcare organizations by downing their reimbursements.
4. The issue of compliance risks in Credentialing
Credentialing in the healthcare delivery systems must meet federal, state, and payer requirements. Refusal to do so can lead to penalties, contract breaches, or legal repercussions. Among others, compliance risks for outsourced IT services can be reduced by implementing regular audits and referring to the current standards when performing the audit.
5. Handling Bulk Credentialing in Healthcare
Groups of healthcare institutions credential multiple providers, and in large organizations, this process could turn into a nightmare if done manually. These processes can be made efficient and devoid of many mistakes by incorporating digital solutions.
6. Failure to meet renewal deadlines in credentialing
Credentialing is not a one-time affair. Providers have to obtain their qualifications anew on a regular basis. Lack of renewal may result in the suspension of privileges that, in a negative way, affects the patient or clients and, at the same time, a financial blow to the organization.
Red Flags for Credentialing in Healthcare
It is important for quality and compliance to identify the early roots of these issues during the credentialing process. These include:
Red Flag | Description |
Gaps in Employment History | Lack of professional activity at times unknown |
Multiple Malpractice Claims | The previous record of claims that are indicative of the risk of malpractice |
Disciplinary Actions | Past actions by medical boards that were punitive |
Inconsistent Credentialing Information | Difficulties with the details furnished |
They should be dealt with before they cause problems, thereby ensuring that credentialing processes are not compromised.

How Credentialing Issues Have Affected U.S. Healthcare
Credentialing issues in healthcare directly influence various aspects of the U.S. healthcare system:
1. Patient Safety and Credentialing
Filtering out the unreliable suppliers of healthcare services decreases the chances of mistakes as well as increases public confidence in hospitals. Credentialing also plays a protective function, ensuring that the provider complies with the required standards of safe and efficient care.
2. Regulatory Compliance and Credentialing
The use of credentialing as a requirement by accrediting bodies in the delivery of healthcare services stabilizes compliance to meet the legal laws and standards governing the delivery of healthcare services and thus prevents any legal attack that would lead to penalties and endanger the reputation of an organization’s healthcare delivery services. The consequences include A cost or expense incurred: A large fine, Adverse business effect on A particular operational aspect.
3. Financial Impact of Credentialing Issues
Credentialing is vital since healthcare organizations will receive corresponding reimbursements from insurance payers as fast and accurately as possible. The reimbursing process plays a role in financial healthcare organizations. I was able to establish that credentialing has a great impact on the cash flow and general operation of a facility.
4. Provider Reputation and Credentialing Standards
The credentialing procedure ensures that the hospital, the patient, and the whole community place their trust in the particular practitioner. Healthcare organizations with sound credentialing processes are considered more credible and trustworthy.
Solutions to Credentialing Challenges in Healthcare
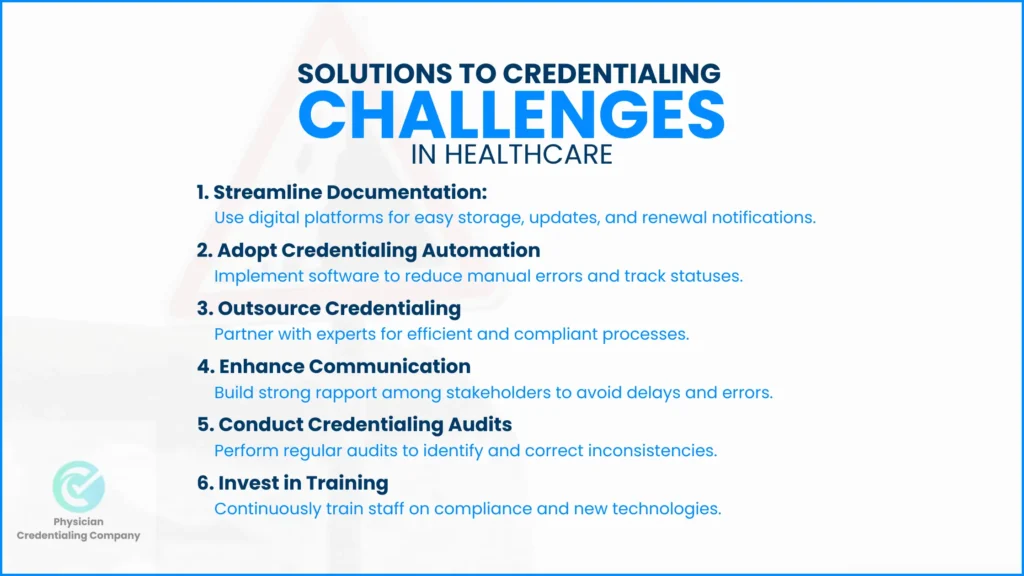
1. Streamlining Documentation for Credentialing
There is a need to adopt recognized and standard approaches in managing provider information with predesignated electronic systems for credentialing storage and updating. This minimizes mistakes and makes it easier to find what is needed. Digital platforms also offer notification for renewal and changes in compliance requirements.
2. Adopting Credentialing Automation
Use electronic software experts to reduce manual input and checks. Automation minimizes data entry and credentialing errors, and it also enables tracking of credentialing statuses.
3. Outsourcing Credentialing Processes
Outsourcing credentialing with specialized service providers helps in addressing payer criteria in an efficient manner. Outsourcing can also facilitate this by bringing in expert know-how and equipment a little quicker.
4. Enhancing Communication in Credentialing
Ensure that there is good rapport between the stakeholders since misunderstandings and delayed notifications may arise in most circumstances. This way the regular update and feedback can help all the parties to be on the same page when in the process of credentialing.
5. Engaging in credentialing form and Credentials file Audits
Originality An important aspect that is encouraged is the periodic audits of credentialing processes so that inconsistencies or errors in it may be noted early and corrections made. These audits guarantee adherence with modification in regulatory frameworks and engender organizational efficiency.
6. Investing in Credentialing Training
Informing staff on credentialing needs and changes also helps them work better and be in compliance. Actually, continuous training makes teams ready for new challenges or helps them adopt new satisfying technologies.
Conclusion
Healthcare credentialing challenges are real and enormous, but four key strategies can help address them. These include; delays, inaccuracies, compliance risks, missing of deadlines which are costly and will have an impact and affect efficiency of the healthcare delivery system. These are real challenges, but by strengthening process efficiencies, promoting the use of innovation technologies, and encouraging organizational interdisciplinary teamwork, healthcare organizations can effectively manage these challenges.
Credentialing cannot be relegated merely as a check on regulatory compliance specifications. It helps to protect the patient, provider image, and financial solvency of the healthcare organizations from potential deception by either the users or providers of the information. Other than addressing continuous issues of physician credentialing as they arise, it is also important to address them preemptively; this way, trust among the patients and other stakeholders is maintained, showing the organization’s acknowledgment of quality services and patient care.
New solutions, such as interaction with organizations and decentralized forms of centralized credentialing systems, have become innovations. These developments reduce human risks and produce quick services through which one can monitor tasks in real-time, thereby reducing healthcare providers’ working loads and unreducible patient attention. Moreover, outsourcing complicated credentialing processes to these outsourcing firms can also help internal teams relieve extra tasks, which may not be easy to manage compliance with various standards that are changing from time to time.
The present-day healthcare delivery systems are dynamic; credentialing must also have to be dynamic in order to meet the present-day challenges. If innovation, collaboration, and the pursuit of ongoing improvement are established as priorities, not only can current credentialing problems be solved, but a strong structure for the future can be built as well. These measures can help credentialing to be a fully efficient, integral, and permanent part of the delivery of quality patient care. Such a strategic approach can also prepare healthcare providers to succeed within the contemporary environment that is becoming progressively crowded and, at the same time, safeguard the interests of people.
FAQs on Credentialing Issues in Healthcare
Credentialing issues shall be understood as the difficulties that may occur during the process of confirmation of the candidature or employee’s compliance with the requirements for his/her education, experiences, and membership in the professional associations. Such concerns could be poor document compliance, history of education and work experience, slow processing of such applications, or differences between claimed and ascertained qualifications. These problems may, in some cases, prevent people from determining whether the healthcare provider is capable of rendering the needed care, and this may have implications for patient safety and care provision.
The three major issues in healthcare are:
Access: This is about the coverage costs to highlight fair access to health services, especially in rural areas where these services are limited.
Quality: Healthcare quality identifies how the healthcare system performs in achieving the standard of safety and efficiency in the delivery of appropriate services to patients. While receiving poor-quality care, a patient is likely to experience some negative outcomes.
Cost: The cost of necessities such as healthcare is constantly increasing as well as treatments, drugs and insurance. Self-employed individuals and families often have to pay significantly more for their care, ensuring healthcare remains accessible regardless of cost is important but often costly for the providers as well as the insurers.
Red flags for medical staff credentialing include:
- Discrepancies in application or background information: Sometimes factual information can be doubtful, for example, frequent or long gaps in employment or education.
- Malpractice claims or adverse actions: Past legal actions and cases against the provider or the license that the provider holds can also put into consideration whether there is something wrong with the competency or the behavior of the provider.
- Failure to meet continuing education requirements: Some of the providers may not have updated themselves with their needed certifications or training. Hence, they may be negligent with current medical practices.
- Lack of valid or current licenses: So, if a healthcare professional does not possess active, valid Licenses in the state or the region where he/she works, then it becomes a major concern.
Credentialing has improved US healthcare by ensuring providers meet professional standards, enhancing patient safety, and maintaining care quality. However, it has also introduced administrative challenges and delays that can affect provider access and efficiency.

