Credentialing is a fundamental process that establishes the qualifications of licensed professionals and assesses their background and legitimacy to provide services. This procedure is crucial in various sectors but is most prominently observed in the healthcare industry, where it helps ensure that medical professionals meet the stringent standards required to deliver safe and competent care. A credentialing process flow chart offers a visual representation of each step involved, clarifying the progression from initial application to final approval, and is an essential tool for administrators and oversight committees tasked with overseeing this meticulous process.
The flowchart simplifies the complexity of credentialing by breaking down the process into discrete, manageable steps. It begins with the gathering of professional records and information, which includes education, training, licenses, certifications, and work history. The subsequent stages involve primary source verification of the provided information, committee reviews, and ongoing monitoring to uphold compliance with industry standards. Throughout this process, documentation plays a pivotal role, ensuring a traceable and transparent pathway for each credentialing case.
Information systems have evolved to support the credentialing process, enabling more efficient data management and improved accuracy in verifying qualifications. These systems facilitate the tracking of performance metrics, which are critical for timely renewals and re-credentialing. In addition, they assist in identifying and addressing any delays or issues that arise, ensuring that the credentialing process aligns with current and future trends, regulations, and best practices. The incorporation of a behavioral health credentialing flowchart can be particularly beneficial for managing the unique requirements and complexities associated with mental health services.
Key Takeaways
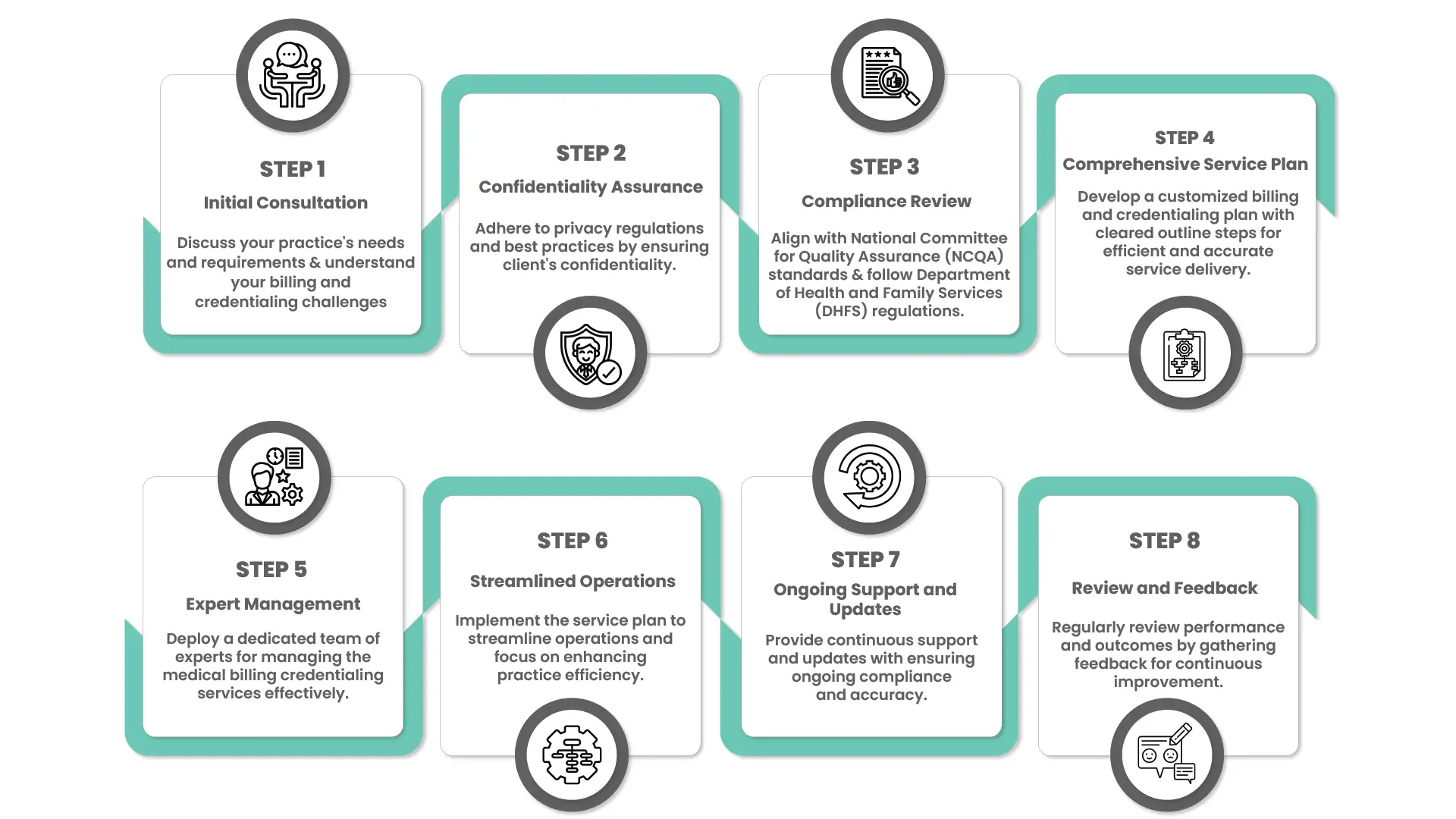
- An infographic representation of Credentialing Process Flow chart for a quick idea.
- Credentialing validates the qualifications and backgrounds of professionals.
- A flowchart delineates the steps, from data collection to committee approval.
- Information systems are integral to managing and optimizing the credentialing process.
Visual Credentialing Process Flow chart
For better experience, we have also created an infographic credentialing process flow chart for your ease if you would like to get a quick idea.
Credentialing Basics
The credentialing process is a critical procedure ensuring medical professionals have the necessary qualifications to provide healthcare services.
Definition and Importance
Credentialing is the verification of a healthcare provider’s qualifications to ensure they meet the necessary professional standards. It is crucial in maintaining patient safety and high-quality care. During this process, credentials such as education, training, and board certifications are rigorously checked against established industry standards.
Key Participants and Stakeholders
- Healthcare Providers: The individuals who undergo the credentialing process.
- Credentialing Committees or Departments: They conduct the review and verification of the provider’s qualifications.
- Insurance Companies: They require credentialing for providers to join their networks.
- Medical Facilities: They ensure only qualified providers practice within their institutions.
- Patients: Indirect stakeholders who rely on credentialing to assure quality care.
Credentialing Steps
The credentialing process is a rigorous and structured sequence that ensures healthcare professionals are properly qualified and legally permitted to provide care.
Initial Data Gathering
The Initial Data Gathering phase involves collecting comprehensive information from the healthcare professional seeking credentialing. This includes their educational background, work history, licenses, certifications, and any specialty credentials. A checklist is often utilized to ensure no critical piece is overlooked.
- Education: Gather diplomas, transcripts, and training certificates.
- Work History: Compile past employment details, highlighting healthcare roles.
- Licensing: Collect current state or national medical licenses.
- Certifications: Obtain relevant board certifications or specialty qualifications.
Primary Source Verification
In the Primary Source Verification stage, the information gathered is verified directly with the primary sources. This step is critical to confirm the accuracy and authenticity of the professional’s credentials.
- Education Verification: Contact educational institutions to confirm degrees and training.
- License Verification: Check with licensing boards to ensure the validity and status of medical licenses.
- Work History Verification: Confirm employment history with previous healthcare employers.
- Certification Verification: Authenticate board or specialized certifications with the issuing organizations.
Credentialing Committee Review
The Credentialing Committee Review involves a panel of experts who thoroughly evaluate the verified credentials against established standards. They assess the candidate’s qualifications and determine if the candidate meets the necessary criteria to proceed.
- Qualifications Assessment: Review and assess the professional's qualifications.
- Meeting Standards: Ensure the candidate meets set healthcare standards.
- Committee Deliberation: Discuss findings and form a consensus on the candidate's suitability.
Board Approval
Finally, the Board Approval step takes place. The committee’s recommendation is presented to the governing body or board, which makes the final decision on the healthcare professional’s credentialing status.
- Recommendation Review: The board examines the committee's recommendation.
- Final Decision: The board grants or denies credentialing based on the provided evidence.
Each of these phases is interconnected and essential to a successful credentialing process, guaranteeing only qualified individuals are approved to practice within healthcare institutions.
Documentation and Compliance

The “Documentation and Compliance” phase in the credentialing process is essential for ensuring that healthcare professionals meet all necessary standards and maintain adherence to regulatory requirements.
Required Documents Checklist
To begin credentialing, a comprehensive checklist of required documents is necessary. These documents typically include:
- Professional Licenses: Verification of current state medical licenses.
- Board Certification: Proof of board certification in the healthcare provider's specialty.
- Work History: Complete work history, including any gaps in employment.
- Education and Training: Transcripts and certificates from medical schools and residency programs.
- References: A list of professional references, preferably from the medical field.
- Proof of Identity: Government-issued photo ID (e.g., passport or driver's license).
Standards and Regulations
Healthcare providers must comply with a rigorous set of standards and regulations. The standards often revolve around:
- Accreditation: Adherence to standards set by bodies like The Joint Commission or NCQA.
- State Laws: Each state may have unique legal requirements for practicing healthcare professionals.
- Federal Regulations: Compliance with federal laws, including but not limited to HIPAA and OIG.
Continuous Compliance
For healthcare practitioners, maintaining compliance is an ongoing responsibility. They must ensure:
- Credential Updates: Timely renewal of licenses, certifications, and other credentials.
- Training: Participation in continuing education to stay abreast with the latest medical advancements and regulatory changes.
- Audit Readiness: Keeping documentation updated and readily available for periodic audits.
Information Systems in Credentialing
Information systems play a crucial role in streamlining the credentialing process. They ensure accuracy and efficiency in managing healthcare professional credentials.
Credentialing Databases
Credentialing databases are specialized software solutions that store and manage healthcare providers’ qualifications, certifications, and other pertinent professional documents. These powerful databases support the verification of credentials by aggregating data from primary sources and presenting it in an accessible format. They often include:
- Profiles of Healthcare Providers: Listing educational history, training, and board certifications.
- Verification Records: Documenting source verification of licenses, DEA certificates, and malpractice claim history.
- Document Management: Enabling secure storage and easy retrieval of credentialing documents.
Credentialing databases enhance the integrity of the credentialing process by providing a singular point of truth.
Process Automation
Process automation in credentialing involves the use of software to automate repetitive and time-consuming tasks. These tasks may include:
- Primary Source Verification: Automatically sending verification inquiries to licensing boards and educational institutions.
- Alerts and Notifications: Sending reminders for upcoming expirations of credentials and required actions.
- Workflow Management: Assigning tasks and tracking the progression of the credentialing process.
Automation reduces the potential for human error and helps maintain compliance with industry standards and regulations.
Performance Monitoring and Reporting
This section provides a detailed overview of the mechanisms in place to track and report the efficacy of the credentialing process.
Key Performance Indicators
Key Performance Indicators (KPIs) serve as quantifiable measures to assess the success of the credentialing process. Common KPIs include:
- Time to Credential: The average duration it takes to complete the credentialing process for a provider.
- Credentialing Accuracy: The percentage of applications processed without errors.
- Compliance Rate: Alignment with regulatory and policy requirements.
Regular Reporting Procedures
Proper reporting is essential for maintaining the integrity and accountability of the credentialing process. Institutions typically adhere to the following reporting procedures:
- Monthly Reports: A summary of credentialing activities, delivered monthly to management.
- Audit Reports: Periodic detailed reviews of the credentialing process, highlighting any discrepancies.
- Stakeholder Updates: Regular briefings provided to relevant parties, including department heads and regulatory agencies.
Recredentialing Process

The recredentialing process is vital to maintain the standards and compliance within healthcare facilities. It ensures practitioners continue to meet the necessary professional requirements since their initial credentialing.
Timeline and Triggers
Triggers for recredentialing include the expiration of a clinician’s credentials or mandated review periods by regulatory bodies. The process should start:
- 120 days before the credential's expiration date.
- Upon change of the practitioner's status or scope of practice.
Recommended Timeline:
- Months 5-4: Initiate recredentialing notification.
- Months 3-2: Collect and verify updated documents.
- Month 1: Review and decision by credentialing committee.
Procedures and Documentation
The recredentialing procedures require attention to detail and thoroughness:
- Send notification to the practitioner.
- Receive and review completed recredentialing application and attestation.
- Verify: licensure, malpractice insurance, board certification, Continuing Medical Education (CME) credits.
- Query: National Practitioner Data Bank (NPDB).
- Conduct Primary Source Verification (PSV) for all credentials.
Required Documentation:
- Current professional license.
- Proof of malpractice insurance.
- Evidence of board certification and CMEs.
- Updated curriculum vitae (CV).
- Health and immunization records, if applicable.
Documentation should be organized and stored securely, respecting privacy and confidentiality requirements.
Handling Delays and Issues

In the credentialing process, timely responsiveness to delays and efficient resolution of issues are critical to maintaining workflow integrity.
Common Credentialing Challenges
| Title | Description | Examples |
|---|---|---|
| Incomplete Applications | Often, applications lack necessary information, causing delays. | Missing transcripts or licenses. |
| Verification Backlogs | Primary source verification can face backlogs due to high volume or slow response times. | Difficulty in verifying educational history. |
| System Errors | Technical issues with credentialing software can stall the process. | Database outages preventing application processing. |
Mitigation Strategies
| Title | Description | Example |
|---|---|---|
| Streamlined Communication | Implementing clear channels for applicants to submit missing items. | Tools: Use of checklists and automated reminders. |
| Priority Queues | Establishing a system to prioritize urgent verifications. | Criteria: Time-sensitive applications or those nearing the deadline. |
| Technical Support | Ensuring robust IT support to quickly address system errors. | Action Plan: Regular system maintenance and a dedicated IT response team. |
Future Trends in Credentialing
Credentialing is evolving rapidly, influenced primarily by technological advances and changing regulations. These developments are poised to streamline processes and enhance compliance and accuracy in credential verification.
Innovations and Technologies
Technological advancements are set to transform the credentialing landscape. Among the most prominent innovations are:
1. Blockchain Technology
It promises enhanced security and transparency in the storage and verification of credentials.
- Decentralization: Ensures no single point of failure.
- Immutable Records: Guarantees the integrity of credential data.
2. Machine Learning and AI
These tools are being integrated to automate and accelerate the credentialing process.
- Data Processing: Swiftly analyzes and verifies large volumes of credentials.
- Pattern Recognition: Identifies discrepancies in credentialing information promptly.
Policy Changes and Implications
Changes in legislation and policy are equally crucial in shaping the future of credentialing. Key policy shifts include:
1. Increased Regulation
There is a trend towards stricter regulatory standards for credential verification to prevent fraud.
- Stricter Compliance: Requires robust systems for ensuring credentials are up to standard.
- Regular Audits: Mandates periodic reviews of the credentialing process for compliance.
2. Interstate and International Standardization
Efforts are being made towards standardizing credentialing across jurisdictions to facilitate workforce mobility.
- Uniform Standards: Aims to simplify the recognition of credentials across borders.
- Reciprocity Agreements: Encourages seamless credential verification between states and nations.

