Provider enrollment and credentialing are essential processes within the healthcare industry, pivotal to establishing the legitimacy and qualifications of healthcare providers within insurance networks. These steps are critical for both new and existing practitioners aiming to ensure that they can offer care to a wider patient base and secure proper reimbursement for their services. Credentialing is the initial phase, whereby insurance companies and healthcare institutions verify a provider’s professional qualifications, including education, training, residency, licenses, and any specialty certificates.
Closely linked to credentialing, provider enrollment is the formal process where a provider joins an insurance network. This involves submitting detailed applications and supporting documents to become an in-network provider. Credentialing with Insurance Companies is crucial because it allows providers to bill insurance companies for services rendered to insured patients. Successful enrollment benefits both patients and providers. Patients gain broader access to healthcare services within their network, while providers experience a streamlined reimbursement process for the care they deliver. The accurate and careful execution of both credentialing and provider enrollment is essential for maintaining a high-quality, trustworthy healthcare system.
Understanding the difference between these two processes can be highly beneficial for healthcare providers looking to navigate the complexities of insurance networks. While often used interchangeably, credentialing and enrollment serve separate but complementary roles in a provider’s professional lifecycle. Their execution can significantly impact a provider’s ability to deliver patient care and manage the financial aspects of their practice.
Overview of Provider Enrollment
Provider enrollment is an integral part of the healthcare industry, wherein healthcare providers establish formal affiliations with insurance networks. This process is a prerequisite for providers to receive reimbursement for services rendered to insured patients. It involves submitting detailed applications to each insurance payer with whom the provider wishes to be in-network.
The provider enrollment process can generally be broken into multiple phases:
- Application Submission: Providers submit their personal and professional information to insurance companies for consideration.
- Credentials Verification (which differs from provider credentialing): The submitted information is rigorously verified for accuracy and completeness.
- Contract Negotiation: Upon successful verification, providers may enter into negotiations with payers regarding the terms of their participation in the network.
During enrollment, the following documentation is typically required:
- Professional licenses
- Malpractice insurance
- Past work history
- Educational background
- Board certifications
Successful enrollment is confirmed when a provider receives an effective date from the insurance payer, indicating that they are now participating in the network and can bill for services covered under the plan. It’s a structured process aimed at maintaining the standard of care by allowing only qualified providers to offer services to the payer’s members. This step is a foundational element in ensuring the integrity of the healthcare system by taking a thorough look at the providers’ qualifications.
Failure to maintain accurate and up-to-date enrollment may result in claim denials and interruption of provider reimbursement, making it essential for providers to manage their enrollment status diligently.
Credentialing Process
The credentialing process is essential for ensuring that healthcare providers meet all necessary regulatory and industry standards before joining a healthcare organization or insurance network. Also read about the verification process here.
Verification of Qualifications
The first step in the credentialing process involves rigorous verification of qualifications. Education, training, residency, board certifications, work history, and licenses are meticulously checked. Entities involved in this verification process include medical schools, licensing boards, and past employers to ensure all information provided by the provider is accurate and current.
Provider Background Checks
Background checks are an integral part of credentialing. Healthcare providers undergo thorough background checks that look into criminal history, malpractice claims, and any disciplinary actions taken by licensing boards or healthcare institutions. This step serves as a safeguard, preserving the integrity of the medical profession and protecting patient welfare.
Medical Credentialing Steps
Credentialing includes various critical steps to evaluate if a provider is qualified to deliver care and receive payment from insurance networks. Documentation collection, primary source verification, committee review, and ongoing monitoring of the provider’s performance and compliance with medical standards are among these steps. The process is designed to be systematic and comprehensive to maintain high standards within healthcare services.
Maintaining a clear and methodical approach to credentialing helps to prevent mistakes that could affect both patient care and healthcare organizations’ operational effectiveness.
Enrollment with Payers
Enrollment with payers is a crucial step that healthcare providers take to be recognized by insurance networks. It involves providing necessary details and documentation to insurers for the purpose of billing and reimbursement.
Medicare and Medicaid Enrollment
Medicare and Medicaid enrollment is mandatory for providers who wish to serve beneficiaries under these government-sponsored programs. The enrollment process requires completing specific forms and meeting defined criteria. For example, Medicare necessitates an active license to practice in the state and a completed CMS-855 form. Enrollment ensures providers are officially recognized by these programs and can receive payment for services rendered to covered individuals.
Private Payer Enrollment
With private payer enrollment, healthcare providers must adhere to differing requirements set by various commercial insurance companies. Each company has its own application procedure, which often includes verifying credentials such as education and board certifications. Timing is a factor as well, with the process taking anywhere from a few weeks to several months. Providers must ensure they submit accurate and complete information to facilitate a smooth enrollment with entities such as UnitedHealthcare, BlueCross BlueShield, and Humana. Completing this process successfully enables providers to offer services within these insurance networks and bill for their services.
Regulatory Compliance
In provider enrollment and credentialing, regulatory compliance involves adhering to rules set by governmental bodies and healthcare organizations. Providers must ensure their operations meet these requirements to maintain legitimacy and avoid legal repercussions.
Government Regulations
Provider enrollment and credentialing are governed by a range of government regulations. Healthcare providers must comply with federal laws such as the Health Insurance Portability and Accountability Act (HIPAA), which safeguards patient data. Additionally, they are required to align with the standards of the Centers for Medicare and Medicaid Services (CMS) if they wish to participate in these federal programs.
- HIPAA compliance: Ensures confidentiality, integrity, and security of patient health information.
- CMS requirements: Mandatory for participating in Medicare and Medicaid, including accurate provider data and revalidation every five years.
Compliance with Healthcare Standards
Besides government regulations, healthcare providers must comply with industry standards and best practices. These often include:
- The Joint Commission: Providers align with accreditation requirements that signify quality and safety in patient care.
- National Committee for Quality Assurance (NCQA): Adherence demonstrates commitment to high-quality health care and continuous improvement.
Credentialing Committees play a pivotal role, evaluating providers against the organization’s standards and regulations. Proper compliance ensures that providers maintain their eligibility to offer services and receive reimbursement from insurers.
Maintenance and Re-Credentialing
Maintaining accurate provider data is crucial for ensuring ongoing eligibility for payment from payers and for meeting compliance standards. Re-credentialing, a systematic process typically carried out every two to three years, ensures providers continue to meet the standards set by healthcare organizations and insurance networks.
Key Steps in Maintenance and Re-Credentialing
- Notification: Providers receive notice when it’s time to update their credentials.
- Documentation Update: Providers must submit current documents, including licenses and certifications.
- Data Verification: Information provided is verified for accuracy.
| Action | Purpose |
|---|---|
| Timely Updates | Avoid lapses in payer network participation. |
| Ongoing Monitoring | Ensure compliance with healthcare standards and legal requirements. |
| Periodic Audits | Assess and confirm the validity of credentials on a regular basis. |
The re-credentialing process often involves primary source verification of a provider’s credentials, which may include:
- Medical education
- Board certifications
- State licenses
- Work history
- Malpractice claims history
Providers and healthcare entities should be attentive to credential expirations and initiate re-credentialing well in advance to avoid a lapse in provider status, which can impact patient access to care and provider revenue. Effective systems and a scheduled approach to credentialing maintenance are instrumental in this periodic process.
Technology in Enrollment and Credentialing
The integration of technology has become essential in streamlining the provider enrollment and credentialing processes, enhancing accuracy, speed, and security.
Credentialing Software Solutions
Credentialing software solutions have been transformative, automating tedious tasks and managing large volumes of provider data efficiently. Key features typically include:
- Automated Tracking: Track application statuses, renewal dates, and deadlines.
- Document Management: Store and organize essential documents in a centralized location.
- Verification Support: Facilitate primary source verification with integration to various data sources.
This technology often supports compliance with industry regulations and assists in maintaining up-to-date provider information. Solutions from companies like QGenda optimize these processes, addressing needs like financial uncertainty and patient care standards.
Data Security in Credentialing
The sensitive nature of provider data demands stringent data security measures within credentialing platforms. Significant elements include:
- Encryption: Protecting data both at rest and in transit.
- Access Controls: Defining user permissions to limit access to sensitive data.
Providers and organizations that engage in provider enrollment and credentialing must ensure these systems comply with regulations like HIPAA to safeguard personal and professional information from unauthorized access or breaches.
Difference between Provider Enrollment and Credentialing
Provider Credentialing
Credentialing is related to provider enrollment, as providers cannot be enrolled without medical credentials. If a qualified practitioner submits an application to join a network under a payer, credentialing ensures that claims aren’t rejected. The Steps are:
- Application Evaluation Making necessary files and reporting exceptions.
- Primary Source Documentation: Verify practitioner/ facility information from physicians.
- Outbound Call Center: Identify lost documents and update the payer database.
- Follow-up with payers: Follow-up on submitted credentialing requests.
- Data Entry: Image capture, label, and associate to provider/ facility in the payer’s system.
- Maintenance of Provider Data: Complete policy/procedures and update provider information and CAHQ profile.
Provider Enrollment
Provider Enrollment Services help practices enroll in the services they offer by providing payers with the information they need to issue claims on the services you offer. The payers are a continuous source of interest, and we keep a close eye on and process applications. The procedure is as follows:
Verification of Provider Information
Contact payers to check if they have the right provider data on file before we submit claims.
Updating Practice’s Pay-To Address
Ensure and correct the provider pay-to address or billing address.
Enrolling for Electronic Transactions
the team should able to enroll providers for the following kinds of electronic transactions:
- 1. Electronic Data Interchange (EDI)
- 2. Electronic Remittance Advice (ERA)
- 3. Electronic Fund Transfer (EFT) and Bank Deposit.
- 4. CSI
Monitoring Process
A team of very qualified engineers who specialize in performing research and analysis on possible processor functionality gaps.
Steps To Enroll As A Healthcare Provider
Physician Credentialing:
This involves checking the credentials of a physician to ensure their competence, conformance to the needs of the industry, and whether or not they are qualified to render care within a health organization or insurance plan. It is an integral part of making sure doctors are qualified to provide safe and effective care.
Provider Enrollment
It is the practice of registering doctors with insurance companies or health plans so they can receive payment for the services rendered to their patients. After certifying, the physician can register with one or more payer networks to begin being reimbursed.
The process of physician credentialing and enrollment in provider networks are two key steps that every health system must take. Though they are not mutually exclusive, the two mechanisms are interconnected. Provider enrollment: enrolling physicians and hospitals in private and public insurance. Physician credentialing, on the other hand, is a check of the credentials and privileges of a physician to work in a healthcare facility.
Healthcare credentialing is one of the minimum requirements for being eligible as a provider. Insurance companies must establish that a provider is competent to provide care before they can begin billing for care.
Insurance Panel Enrollment
An insurance panel (or “a payer panel,” “an enrollment panel”) is A group of health providers who work (share) with an insurance provider to provide care for enrolled customers. Thus, joining an insurance panel means being certified with that insurance and a participant. Each insurance company or benefit program has an enrollment payer.
When a panel is “closed,” clinicians cannot make an enrollment application to the insurance. In fact, when it is “open,” practitioners and groups can move forward with credentialing with the payer. Insurance panels are usually only active during a timeframe that is strictly defined by the payer. Insurance panel enrollment is essential to join a network of healthcare providers so they can serve insured patients and get reimbursed. This includes credentialing, documentation, contract negotiations, and approval – which can be challenging due to time constraints and multiple insurance carrier relationships.
While each insurance payer or benefit plan differs in its enrollment requirements, generally, the steps go like this:
I. Gather your documentation
Insurance providers must submit a very specific list of documents to insurance companies when completing their enrollment form. These generally (but not necessarily):
- License Information
- Demographics
- NPI and Tax ID
- Taxonomy Code
II. Contact your intended payer’s credentialing office
After gathering all the documentation, it’s important to understand all the possible applications for enrollment. Then, you’d have to determine if a panel is open.
III. Submit your Application
Once you are sure you’ve completed all the required fields on a given enrollment, send your forms to the payer. Afterward, you will have to follow up with the insurance company to make sure your application does not get “forgotten.”
IV. Sign a Contract
When your application is accepted, you just have to submit an enrollment contract to the payer. Check and approve an effective date and your, if applicable, individual provider fee schedule.
Credentialing for Medicaid and Medicare
Obtaining Medicare and Medicaid cards is the key to starting to offer healthcare to patients. Healthcare providers must ensure they get certified with both Medicare and Medicaid to offer the best care possible for their patients. Medicare and Medicaid are two of the most popular public-funded healthcare programs in the US. They offer critical health insurance to millions of people who would otherwise be unable to afford proper medical care. For medical professionals to participate in these programs, they need to be credentialed. In this article, we will look at Medicare and Medicaid credentialing and what providers must know to become eligible for the programs.
Medicare Credentialing
The government health insurance system Medicare typically covers Americans over 65. It also helps some younger patients with impaired or end-stage renal disease. And it’s important because millions of Americans will have affordable health care.
Enrollment Process with Medicare
Here’s how we usually go about it to help you better qualify as a Medicare new provider:
- Get an NPI: Request a National Provider Identifier (NPI) online or via mail.
- Obtain Medical Malpractice Coverage: Purchase medical malpractice coverage and keep a copy of the declaration page.
- Log in to PECOS: Log into the Medicare enrollment system, PECOS, and start.
- Request Documents: Gather documents such as your NPI, state license, CV, and malpractice insurance information.
- Fill out Medicare provider enrollment form: Complete Medicare provider enrollment form in PECOS.
- Seek Support: Medicare phone support can provide you assistance in filling out an application.
- Co-operate with MAC: Work with your Medicare Administration Contractor (MAC) and provide additional information as needed.
- Choose Specialty Designation: If available, choose a specialty designation related to your industry.
- Apply Fee: Pay the application fee required to enroll or re-enroll.
Medicaid Credentialing:
Healthcare providers and providers have to enroll in Medicaid. Medicaid payments require verification. The specific providers who require Medicaid credentialing are:
- Physicians (MD, DO)
- Dentists
- Nurse Practitioners
- Physician Assistants
- Therapists (Physical, Occupational, Speech)
- Social Workers
- Mental Health Counselors
- Nurses
- Home Health Agencies
- Clinics
- Hospitals
- Laboratories
- Durable Medical Equipment (DME) Service Providers.
If the provider is Medicare/private insurance-covered, they must still credential separately for Medicaid.
Eligibility Criteria for Medicaid Credentialing
- Providers must be the following to be eligible for Medicaid credentialing:
- Possess a current, unlicensed professional license in their state of practice.
- Possess a National Provider Identifier (NPI) number.
- Receive a Tax ID Number (TIN) or Social Security Number (SSN).
- Have all the necessary education, training, and certifications.
- Have cleared a background check and are not excluded from federally funded programs.
- Maintain offices in the state(s) where they apply for Medicaid.
- Complete any other state enrollment requirements.
Credentialing Verification Process
The Credential Verification Process is one of the main processes in ensuring the reliability of all systems from educational to work and special services. It involves carefully checking a person’s credentials, training and professional credentials against purported documents or statements. This process protects the institution from false claims and ensures that they have the relevant skill and expertise claimed. Accuracy and efficiency of verification can be guaranteed only by an organized process of verification.
Companies tend to do so by steps that involve gathering relevant documentation or evidence of credentials. These could be transcripts, certificates, licenses, or reference letters that are checked critically for authenticity. This process of obtaining a credential is generally like this:
- Application Submission: The applicant (e.g., physician, nurse, or other health care worker) files an application with personal data, schooling, credentials, work experience, certificates, and so forth.
- Document Review: The certifying organization checks the submitted documents to make sure that all necessary information is correct, complete, and meets the standards.
- Verification of Credentials: The certification agency calls directly educational institutions, licensing authorities, former employers, and certification organizations to validate the information provided. This can include checking the individual’s training, credentials, licensure, training, board certifications, malpractice insurance, employment history, and so forth.
- Background Check: An employee is checked for criminal record, misdemeanors, and occasionally credit scores to determine his or her work ethics and danger levels.
- Review of Clinical Competence: It may require evaluation of the healthcare practitioner’s clinical abilities and performance, both through peer review and performance reviews, to determine if they can demonstrate the standards of practice. When the authentication is complete, the certification authority will determine it. As long as the person meets the requirements, the credentials or privileges are granted, otherwise the person is denied or requested to explain himself or herself more fully.
- Ongoing Monitoring: This isn’t a one-time requirement. Healthcare workers must stay in compliance through continuous education, renewals of licenses, and re-credentialing at intervals (every 2-3 years or so).
Generally, the qualification process varies slightly from organization to organization, but the idea is always to make sure the individual is competent, capable, and reliable to provide care or services of their profession.
Credentialing for Group Practices
Crediting a practice collectively keeps the enrollment rolling even as providers change. It is more efficient for stable group practices since it does not require administrative hassle to re-credential after each provider’s exit. Credentialing in a collective offers more stability. If a provider exits, your insurance contracts will remain intact since credentials are carried on with the practice. This is particularly useful in eliminating the paperwork and costly re-credentialing hassles.
Authorize a Group Practice Step by Step
Listed below is a simplified, step-by-step process for credentialing a group practice with real-world examples from insurance payers.
Complete the Provider Onboarding Form
This usually involves a completed W-9 form, each provider’s license, proof of malpractice insurance, and the group Tax ID. You should be sure to upload a Provider Roster for every provider listed with the group’s Tax ID and Billing NPI.
Submit Required Documentation
Each insurance payer has their own onboarding. BCBS of Texas, for instance, will need a Provider Onboarding Form that contains information about the group and individual providers. Verify that all details, such as Tax ID and NPI numbers, are aligned with your billing information.
Create and Update CAQH Profiles
Many insurers use the CAQH database to automate credentialing. To prevent credentialing delays, update each provider’s CAQH profile, including credentials and certifications. Make sure you have access to every provider profile.
Stay Organized
Monitor every provider’s applications, follow-ups, and paperwork. It is important to maintain consistent communication with the insurance companies so that the processing is not delayed.
Address Individual Credentialing Needs
Some providers may need to be credentialed as an individual even if they’re part of a team. This is useful for practitioners that can operate in more than one practice
Final Words
Provider credentialing is also a requirement for delivery of care services to patients. In addition, providers can also expand their network and recruit more patients to their practice. Physicians Revenue Group, Inc. provides credentialing and healthcare enrollment for US physicians. Our credentialing specialists take care of all documentation. This allows partner providers to start practicing and servicing more payers.
FAQ - People Also Asks
The provider enrollment process is integral to healthcare operations as it establishes the legitimacy and qualifications of providers, ensuring they meet the standards of payers and regulatory bodies, which in turn maintains the integrity and quality of healthcare services offered to patients.
Credentialing is a process to verify if a medical specialist has the qualifications to provide patients with superior medical care. It’s useful for medical billing software and RCM systems, as the reimbursements are issued quickly without any problem.
Credentialing entails verifying a provider’s qualifications including their education, training, and professional experience. The standard credentialing process typically involves the collection of necessary documents, primary source verification, committee review, and finally, approval or denial.
A provider enrollment specialist focuses on enrolling practitioners in health insurance networks, ensuring compliance with payer requirements. In contrast, a credentialing specialist is mainly responsible for verifying the qualifications and professional history of healthcare providers to make sure they meet the necessary standards for patient care.
Credentialing refers to the process of verifying a provider’s qualifications and background, while paneling is the step that follows, involving a provider’s addition to an insurance network, allowing them to serve a wider patient base and bill for services rendered.
To complete insurance panel credentialing, providers must not only have proper licensure and certifications but also meet specific criteria set by the insurance panel, which may include a clean practice record, acceptable malpractice history, and adherence to the insurers’ coverage policies.
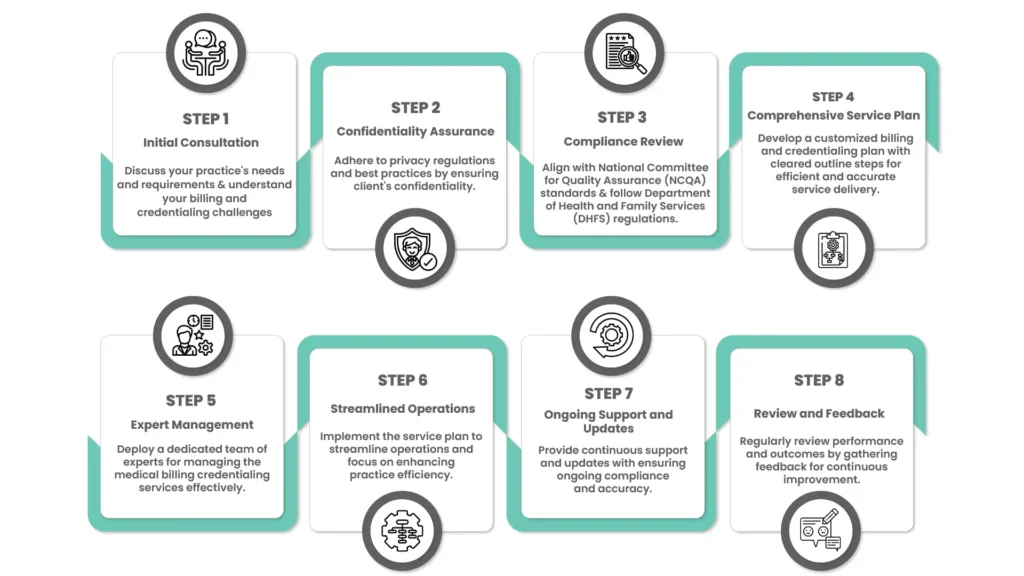
A provider enrollment process flowchart illustrates a step-by-step approach to credentialing, starting with the initial application and culminating in the provider’s acceptance and ability to bill the insurance. It serves as a visual guide, detailing the progression through various stages such as data verification, committee reviews, and final decision-making.
Medical credentialing is the necessary procedure to verify a medical practitioner. In the meantime, payer enrollment asks for coverage within a health insurance network to act as a provider.
Provider credentialing is an important part of healthcare. It involves checking a physician’s experience and credentials to ensure they meet certain insurance companies’ requirements.